Lecture Details[]
Wayne Hodgson; Week 4 MED1022; Pharmacology
Lecture Content[]
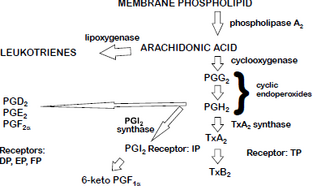
Typical inflammatory response: redness, swelling, heat, pain, loss of function. Autacoids are local hormones; histamine, serotonin, eicosanoids, bradykinin. Neuropeptides are cytokines, complement components, platelet activating factor, oxygen derived free radicals. Uncontrolled pain diminished quality of life; acute has identifiable cause, chronic can be unidentifiable. Eicosanoids are breakdown products of cellular membranes (phospholipids), many of which potentiate pain. Eicosanoids include prostaglandings, thromboxane, prostacyclin (PGI2) and leukotrienes (LT) (lipoxygenase). Eicosanoid produce depends on parent fatty acid, enzymes present. They're involved in uterine motility, bronchodilation/constriction, vasocontriction/dilation, inflammation, gastric ulcers, allergic response. They sensitise afferent C fibres, vasodilate for heat, fever from CNS action, swelling due to increased capillary permeability; synergises with histamine, bradykinin.
Symptomatic pain involves simple analgesics, NSAIDs, morphine-like drugs, local anaesthetics. Simple analgesics are aspirin (300mg; 500 is extra strength), paracetamol (500mg), ibuprofen (200mg); dispirin, aspro, aspro clear; panadol, tylenol, dymadon; nurofen, brufen, parafen. Aspirin and paracetamol can be combined to codeine phosphate.
Mild/moderate pain can be dental pain, period pain, headache. Can also be used for antipyretic, platelet aggregation is not affected by paracetamol but is by aspirin and ibuprofen. Migraine and arthritis are also indicated; side effects are increased bleeding time, peptic ulcers, exacerbation of asthma.
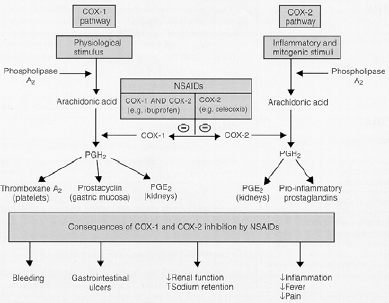
Other NSAIDs are naproxen, mefenamic acid, ketoprofen, diclofenac, piroxicam, diflusinal, indomethacin, sulindac (all MSK). PGE/PGI inhibit gastric acid secretion, enhance mucosal blood flow, promote mucus secretion. Platelets have increased bleeding time, GIT blood loss (3-8ml a day). Allergies are exacerbated by use of leukotrienes. Effects are predominantly due to inhibition of COX which usually allows arachiodonic acid to turn into prostaglandins
COX 1 is involved in housekeeping (platelet aggregation, vascular flow), COX 2 with inflammatory cells. Selective COX 1 is low dose aspirin (good in heart patients), nonselective is high dose aspirin, most other NSAIDs. Selective COX 2 is celecoxib, rofecoxib, meloxicam. There is a lower risk of GIT effects, greater risk of CV events.
NSAIDs enter the hydrophobic channel of cells and form reversible hydrogen bonds preventing FA's from entering, COX2 agents are too big to enter COX1, COX2 side pocket accomodates larger molecules.
Aspirin travels through the liver with a 30% first pass effect to become salicylic acid. t1/2 is 2-4 hours low dose, 15-30 high dose. Irreversible inhibition of COX. pKa of 3.5. Effect depends on dosage- antiplatelet is 0.5-1mg/kg, analgesic/antipyretic 5-10mg/kg, anti-inflammatory >30mg/kg. Can cause salicylism: tinnitus, deafness, headache, mental confusion, convulsions, coma, death. Treated with charcoal, emesis, alkaline diuresis.
Paracetamol only blocks COX2/3, no gastric side effects, no anti-inlammatory action, overdose (>100mg/kg) associated with severe liver damage. Useful when aspirin is contraindicated. Conjugated to glutathione, water soluble and excreted in this state. Excess drug is oxidised to toxic metabolite which denatures proteins. Antidote is the precursor of glutathione (N-acetylcysteine).