Lecture Details[]
IR Young; Week 1 MED2031; Physiology
Lecture Content[]

Inspiration is active, uses muscle force, expiration is passive. Expiration usually takes 2-3 seconds while inspiration takes 1-2 seconds. Intrapleural pressure is -4mmHg, intrapulmonary pressure is 0mmHg, collapsing force of lungs is 4mmHg. Transpulmonary pressure is the pressure difference between the pleural and the alveolar pressure. This is a measure of the net collapsing force, or recoil pressure.
Compliance is a measure of how easy it is to stretch the lungs during inflation. C = change in volume/change in pressure. Compliance change between inspiration and expiration is hysteresis. It is usually about 200mL air/cm H2O for both lungs together. In saline solution, there is less compliance, alveolar air-liquid interface is necessary for increased compliance. Surface tension tends to collapse a spherical structure. There are three types of work necessary to be done in inspiration- compliance work to expand the lungs, tissue resistance work to expand the lungs, and airway resistance work. The chest wall adds further resistance, with the compliance work of the lungs and chest being about double that of the lungs alone.
Elastic forces determining compliance are tissue elasticity due to elastin and collagen fibres (1/3), and surface tension (2/3).
Resistance of airways is dependant on Poisuelle's Law- resistance = constant x length divided by radius^4. Doubling airway radius decreases resistance 16 fold, and halving radius increases resistance 16 fold. A doubling of vessel length leads to a doubling in resistance. On this basis the greatest resistance will be in the smallest airways, but it is actually in the medium size bronchi. The small airways (bronchi) have a large cross sectional area. Medium sized bronchi (over 2mm around the 7th generation) have the highest resistance; low resistance of the smallest airways makes them a silent zone on auscultation. Early obstructive disease affects these vessels first. Surface tension collapses alveoli, smaller ones collapse more than larger ones. Pressure inside alveolus = 2 x surface tension/radius. Surfactant releases surface tension from about 70 dynes/cm to between 5 and 30 dynes/cm. As alveoli collapse, surfactant density increases, stabilising alveolar size.
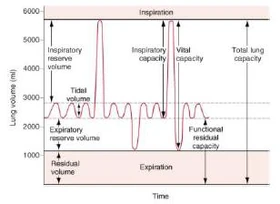
V is volume, V with a dot above it is ventilation. Pa is partial pressure. Dead space can be anatomical (volume of conducting airways, nasal cavity/pharynx and is about 150mL; physiological dead space includes non-functional alveoli can be up to 2L. Measurement of dead space is by measurement of nitrogen concentration (alveolar air has nitrogen, dead air does not). Two main categories of lung disease; obstructive is increased airway resistance, eg asthma; restrictive is reduced lung or thoracic compliance which restricts ability of lung to expand.