Lecture Details[]
Liz Davis; MED1022; Pharmacology
Lecture Content[]
Pathogenic fungi are dimorphic, can be associated with systemic or superficial infections. Pathogenicity is due to allergenicity (inhalation of mold), mycotoxin production (toxins may be inhaled or ingested), tissue invasion. Fungi can be eukaryotic (plant-like but lack chlorophyll, must absorb food from others, don't use light). Can be yeasts or moulds (produce branching hyphae). Mycoses are fungal infections, can be superficial, cutanous (tinea), systemic or deep (involves organs, inhalation) or subcutaneous mycoses which can infect via wound.
Common superficial fungal: oral candida in babies, candidal nappy rash in babies, vaginal thrush (candida), athlete's foot (tinea pedis), other fungal skin infections, onychomycoses (fungal infection of nails). Systemic mycoses can be candidasis, normally present in GIT/vagina, symptomatic infection with broad spectrum antibiotics, immunosuppression, alteration of reproductive tract. Systemic infections can be aspergillosis (pulmonary, invasive, disseminated); candidasis (GI, disseminated), cryptococcosis (meningitis, endocarditis). Aim is chemotherapy and selective toxicity. Predisposing factors are moisture, warmth, broad spectrum antibiotics, diabetes and immunodeficiency.
Major antifungal (selective toxicity) drug groups are cell membrane synthesis inhbitors- azoles, non-azole inhibitors (terbinafine), others (amorolfine); cell membrane disrupters- polyenes (amphotericin, nystatin), cell wall synthesis inhibitors- caspofungin, antimetabolites. Most antifungals are narrow spectrum.
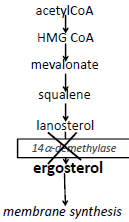
Antifungal drugs target cell membrane (synthesis and integrity), fungal cell wall, fungal DNA synthesis and cell division. Cell membrane contains ergesterol, azoles target synthesis by inhibiting 14-a-demethylase which disrupts phospholipids, inhibits growth and interferes with membrane bound enzyme systems. It is fungistatic.
Azoles are synthetic compounds with broad antifungal spectrum. Topical application gives minimal absorption. Differs in spectrum of activity, pharmacokinetics, adverse effects. Fluconazole penetrates well into the brain, used for fungal meningitis.
Terbinafine also targets ergesterol by targeting squaline epoxidase, can be fungicidal in some species. Terbinafine is active against a wide range of skin pathogens (particularly against nail infections. Used orally to treat nails. Also used topically. Adverse effects after oral administration are rare (reduced WBC, severe skin reactions and hepatotoxicity).
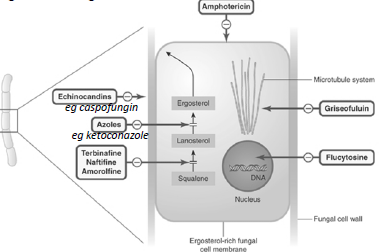
Amphotericin/nystatin targets membrane integrity, polyene antibiotic derived from Streptomyces, binds to ergesterol and disrupts all membranes causing a change in permeability. Larger doses are fungicidal, smaller fungistatic. Amphotericin is drug of choice for disseminated aspergillosis/candida, poorly absorbed from GIT and highly protein bound. Can use for upper GIT, lozenges are used for oral thrush. IV use for systemic fungal infections, can have renal toxicity and other serious effects. Nystatin is similar, only used topically.
Caspofungin targets cell wall synthesis by inhibiting glucan, second line for aspergillosis. Griseofulvin has narrow spectrum of activity, inhibits microtubules and prevents mitosis. Incorporated and concentrated in keratin.